Mom of twins shares warning signs of pregnancy-related heart disease
A New Jersey mom is speaking out about a potentially deadly heart condition she was diagnosed with after giving birth to twins.
Danielle Cognetti said she had a smooth pregnancy, exercising as many as five days per week, until August, when she was forced into emergency labor when one of the baby's vital signs grew concerning.
"I remember the doctor telling me [that day], 'We're going to deliver you,'" Cognetti, who underwent 11 rounds of in-vitro fertilization, told "Good Morning America." "It was a bit of a shock to me."
Cognetti gave birth to her twin daughters, Chloe and Ava, via an emergency cesarean section that day, five weeks before her due date.
During the delivery, Cognetti suffered complications, including hemorrhaging and developing preeclampsia, or extremely high blood pressure.
"I was in a hospital room for 24 hours on this [magnesium] drip, so I was unable to get out of bed or move," she recalled. "They just had to really control the blood pressure to make sure it didn't lead to a seizure."
Cognetti's daughters were placed in the neonatal intensive care unit because of their premature birth.
"Nothing prepares you for the NICU," said Cognetti. "Nobody gives you a warning of exactly what that means, what that looks like, so that too was a bit of a shock."
Cognetti was discharged from the hospital about four days after giving birth, but would soon suffer another shock when she developed symptoms of swelling and difficulty breathing.
"The first night I was home, I was swollen and just really winded and couldn't breathe well," she said. "Again, I attributed everything to I just gave birth and this is probably some natural stuff."

"The second day the swelling was really intense, but then my final straw was I had woken up in the middle of the night to try to go to the bathroom and I just couldn't breathe. I couldn't get to the bathroom and back," she said.
Cognetti put off going to the hospital that night, thinking the symptoms were just related to her delivery, but called her doctor in the morning.
"I was so winded I couldn't even get my story out as to how I was feeling," she said of the phone call. "The nurse on the other end just said, 'Go back to labor and delivery and we'll see what's going on.'"
Cognetti was quickly admitted to the hospital, but even at that point she said she suspected she had COVID-19, not a rare heart condition.
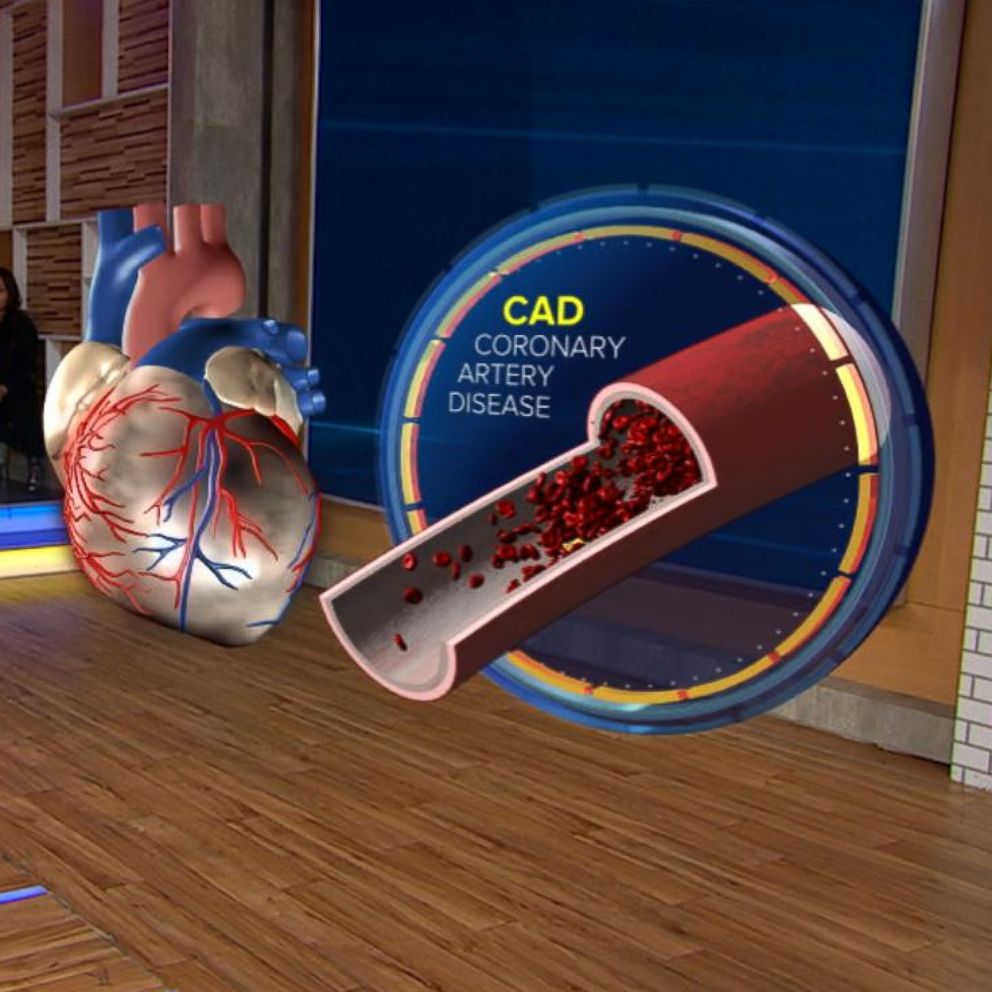
After undergoing a series of tests, Cognetti was diagnosed with peripartum cardiomyopathy, also known as postpartum cardiomyopathy, a rare but potentially deadly disease where the heart muscle weakens. The disease typically occurs during the last month of pregnancy or up to five months after giving birth, according to the American Heart Association.
Cognetti's twin pregnancy and the fact that she is over age 35, considered to be of "advanced maternal age," may have put her at higher risk for the disease.
"It was the shock of my life," Cognetti said of the diagnosis. "I just couldn't wrap my head around it. I could not understand how, you know, how I found myself in heart failure."
Cognetti said she was told by doctors that her heart was working at 35% capacity at the time of her diagnosis.
"It's always heart-wrenching to deliver that news," said Dr. Anu Lala-Trindade, a cardiologist at Mount Sinai in New York City, who treated Cognetti. "I came into her room and had to tell her that her heart muscle function was weak."
Between 1,000 and 1,300 women develop peripartum cardiomyopathy in the U.S. each year. It can be hard to diagnose because its symptoms can "mimic those of third trimester pregnancy," according to the AHA.
There is also no known cause of peripartum cardiomyopathy.
Lala-Trindade said Cognetti's decision to listen to her body and reach out to her doctor helped to save her life.
"I think women oftentimes ignore or downplay their symptoms as not real, or maybe in their head," she said. "Shortness of breath, excessive leg swelling, not being able to breathe when you sleep, these are things that should prompt medical attention."
Depending on the severity of peripartum cardiomyopathy, some women may recover fully or stabilize on medications, while others may suffer severe heart failure, according to the AHA.
Many women recover normal heart function or stabilize on medicines. Some progress to severe heart failure requiring mechanical support or heart transplantation.
"It's so critically important for us to remember that heart disease is the No. 1 killer of women," said Lala-Trindade, citing a statistic from the U.S. Centers for Disease Control and Prevention.
Cognetti was able to stabilize her peripartum cardiomyopathy through a strict regimen of medications and diet.

Doctors may recommend a low-salt diet and fluid restrictions to treat peripartum cardiomyopathy, according to the AHA. Women with the condition are also advised to avoid alcohol and smoking.
Cognetti said she fought hard in her recovery for her daughters, who came home from the NICU two weeks after their birth and are now happy and healthy.
"I remember holding them and saying, and sometimes crying, and just saying that, you know, 'I have to get better for these girls. Like, I cannot believe I fought so hard to have this, and I'm not going to be healthy enough, or worse, I'm not going to be here for them,'" she said. "It's an incredible blessing to have two of them."
Cognetti said she is fearful that her heart disease may flare up again, but she is sharing her story to help other women.
"If I could help another woman out there, or several women out there, notice that if she is experiencing severe swelling, and shortness of breath to please go get help," she said. "Don't make the decision that this is just a side effect of giving birth recently. Let a doctor make that decision for you because it could save your life."